The decriminalization of illicit drug use in B.C. will end Jan. 31, as Minister of Health Josie Osborne admits that the three-year project “hasn’t delivered the results we had hoped for.”
Osborne announced the decision today, explaining that the province will not ask for an extension to the current exemption granted by Health Canada that affects B.C.’s adherence to the Controlled Drugs and Substances Act. Put into effect for a three-year period starting Jan. 31, 2023, the exemption freed people from criminal charges if caught with up to 2.5 grams of an illicit substance, including streets drugs like cocaine, methamphetamine and heroin.
British Columbia was Canada’s first jurisdiction to be given such an exemption, making the province a testing ground for the rest of the country to watch. The exemption was granted as part of a larger movement to help those struggling with addiction get the help they need.
“The decriminalization of people who are in possession of drugs for personal use is one additional step to save lives as we continue to tackle the toxic drug crisis in B.C.,” stated Provincial Health Officer Bonnie Henry when the exemption was granted in 2023. “This exemption will help reduce the stigma around substance use that leads people to use alone and will help connect people to the health and social supports they need.”
Drug overdose has become the most common cause of unnatural death in B.C., surpassing homicide, suicide and car accidents combined. First Nations are affected by the crisis at a rate six times that of the rest of the population, according to the First Nations Health Authority, and in September 2024 the Nuu-chah-nulth Tribal Council declared a state of emergency over the issue.
Decriminalization came at the beginning of a year that would be the most deadly for British Columbia. Over 2023 an average for more than seven people died each day from illicit drug use, with fentanyl detected in 85 per cent of fatalities.
But since 2023 deaths have declined. The B.C. Coroners Service’s latest data from October 2025 shows an average of less than five fatalities a day across B.C., with fentanyl found in 69 per cent of deaths last year.
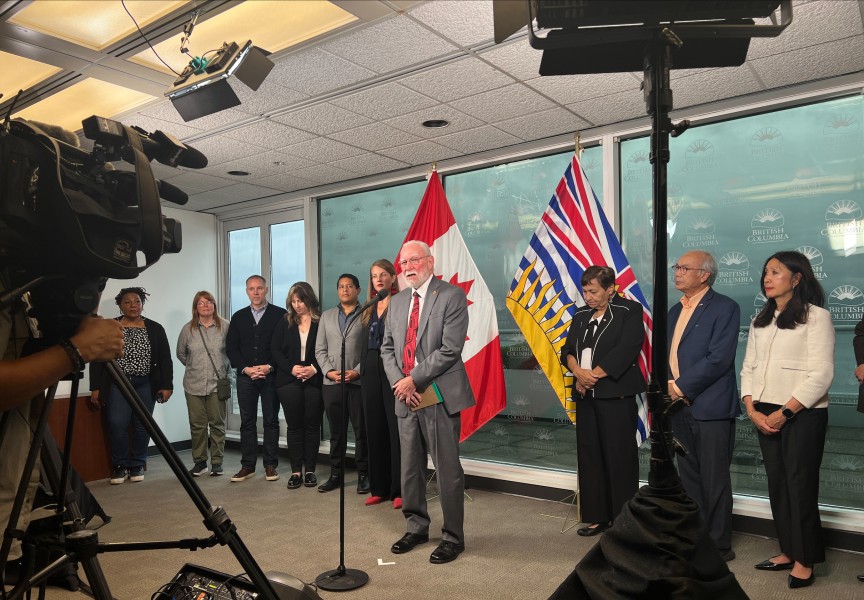
Despite this trend, during a press conference on Jan. 14 Osborne noted that not enough services were being accessed to justify continuing with a policy that allows public drug use, “something that makes almost all of us feel uncomfortable.”
“Ultimately we were not seeing results in the way of a huge increase in self-referrals to care, an increase in certain kinds of services, and the public awareness and understanding that’s necessary creating all the conditions for success,” said the health minister at Victoria’s Royal Jubilee Hospital.
As decriminalization unfolded, it became clear that the province was engaged in a politically risky balancing act: fostering a more welcoming environment for drug users in the hopes of promoting recovery, while managing the discomfort of the greater public in living alongside open-air substance use.
With a fall election on the horizon, the province scaled back its decriminalization policy less than halfway through the project. On May 7, 2024 B.C. received federal approval to again prohibit the consumption illicit drugs in public places, including hospitals, transit and parks, while the 2.5-gram exemption remained for homes, private vehicles and tents. Illicit drug use has always been banned near schools, playgrounds and skate parks.
This scaling back was criticized by the First Nations Health Authority, which cited an increase in arrests. B.C. had an average of 718 possession offences a month from 2019-2022, reported the FNHA, but this declined to 165 monthly arrests after decriminalization began in early 2023. But possession charges rose in the months after May 2024 to an average of 450.
“Arresting people who use substances and putting them through the criminal justice system creates more harm because of the many consequences that make it more difficult to find a pathway to healing,” stated the FNHA in a report from January 2025. “A criminal record can impede the ability to seek employment, housing and may impact access to children and family.”
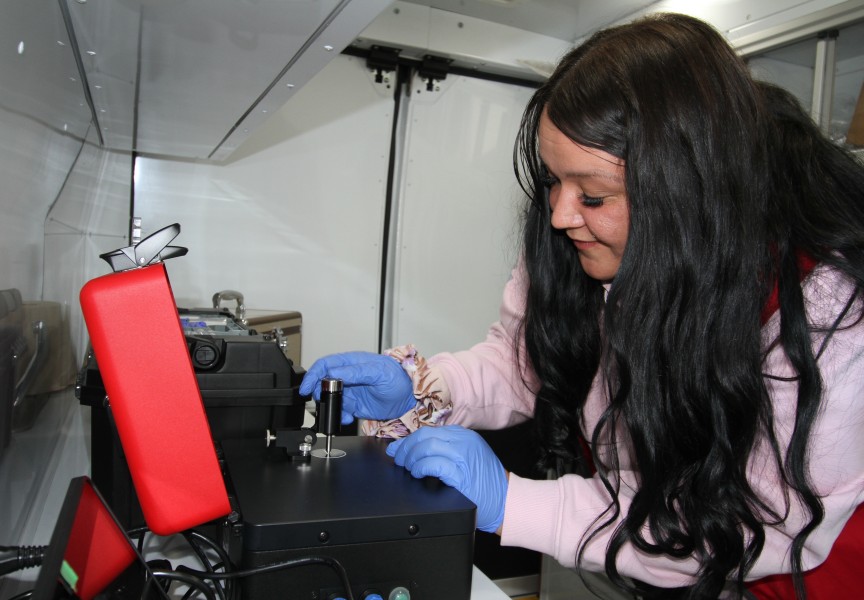
The end of decriminalization will not bring an aggressive crackdown on drug users, said the health minister, as police will, when appropriate, urge people to use their substances in provincially regulated overdose prevention sites rather than public spaces.
“With the end of the exemption, police officers can fully enforce and focus on the most serious offences within the Controlled Drugs and Substances Act,” stated Dwayne McDonald, deputy commissioner and commanding officer of the BC RCMP in a media release. “Police will continue to apply a measured approach to our enforcement efforts, while upholding the safety and security of the communities we live and serve in.”
Telephone service expands to offer rapid response
While addressing the end of the decriminalization project, Osborne announced that a successful telephone service launched in Vancouver over two years ago will now be available to those seeking addictions treatment in other parts of the province. Available in Vancouver since October 2023, Access Central is a clinical telephone service that coordinates addictions treatment. The service offers an assessment from a nurse or clinician within 24 hours, arranging placement in a detox bed or “rapid connection to outpatient services”, said the province. When appropriate, Access Central initiates opioid agonist therapy, like methadone or hydromorphone, or anti-craving meds for alcoholics.
“There is a moment many people in recovery describe, a private, deeply personal turning point when they realize something in their life needs to change,” said Leah Hollins, chair of Island Health’s Board of directors, while announcing the telephone service. “It ensures that when someone reaches out for help, our care team is ready to provide support they need and deserve with dignity and respect.”
Kim Keats, a registered nurse with Access Central, believes that the service will be helpful to those in remote communities.
“I’ve seen people fall through the cracks when access is complicated,” she said. “They have told their stories so many times, and sometimes they’re exhausted before care even starts.”
For those in the Island Health region, Access Central is available seven days a week, from 9 a.m. to 7:45 p.m. at 1-888-885-8824.