Over seven years into British Columbia’s public health emergency, a sobering message on the overdose crisis has come from a nurse who has worked with First Nations for 20 years.
Tanya Dick, a registered nurse with the B.C. Ministry of Health, said that relying on the provincial health care system to treat substance addiction “is like jumping in a boat with holes in the bottom.”
“The systems aren’t built for us, they’re not working for us, and they’re actually contributing to the loss of us,” said Dick, who was among the panelists in an opioid overdose forum held by the Nuu-chah-nulth Tribal Council on Oct. 30 at the Port Alberni Friendship Center. “I personally don’t believe in the bigger health care system right now. I will continue to fight and be a part of it to try and close the gaps.”
As the opioid crisis shows no signs of abating, there appears to be countless systemic gaps, leaving drug users and their families to struggle in breaking the cycle of addiction. Over the first eight months of 2023, 1,645 people in British Columbia were lost to illicit drug use, far exceeding the 995 deaths when the issue became a public health emergency in 2016. Fentanyl has been detected in 82 per cent of fatal cases, according to BC Coroners data from last year.
Aboriginal people have been affected at a rate over five times that of the rest of the B.C. population, says a First Nations Health Authority report from 2022.
The issue has affected Dick personally, as her sister was wrapped up in drug addiction for over a decade in Victoria.
“I spent 10, 12 years, wandering the streets looking for her, finding her once in a while,” said Dick, who is a member of Dzawada'enuxw First Nations of Kingcome Inlet. “Nine times out of 10 I couldn’t convince her to come home.”
But eventually the sister did go home to Kingcome Inlet, where she reached out to family. Now the mother of four has been straight for a few years, and runs a water taxi business in the remote community.
“It was the big house, it was the family, it was the community, it was the nation that helped her find her way back,” said Dick. “If we wait until the government, both provincially and federally, creates a system that’s going to catch us and save us from dying, I think we’re setting ourselves up for failure. We have to, on a parallel level, do that ourselves as nations, as individuals, as families, as communities.”
On Vancouver Island, more help is on the way, according to a provincial announcement issued days before the opioid awareness meeting. Forty more publicly funded treatment beds are coming to the region, including 10 Indigenous focused spots at the Kackaamin Family Development Centre in Port Alberni.
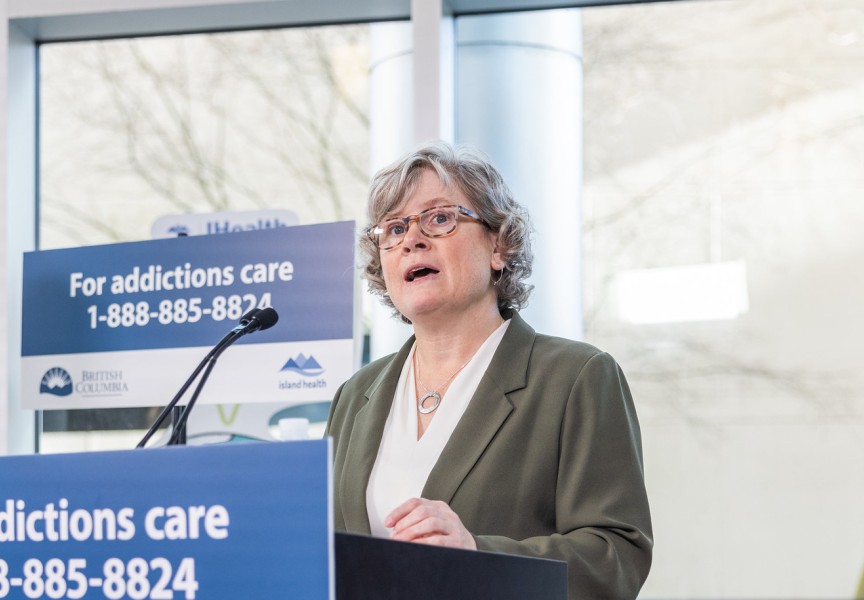
“This represents a significant expansion and investment in substance-use services for clients experiencing dependence on substances including, but not limited to, alcohol or opioids,” said Island Health Board Chair Leah Hollins in a press release. “These are the first publicly funded treatment services of this kind on Vancouver Island. Previously, people would have to travel to the Lower Mainland for this level of intensive treatment.”
It may be an improvement, but the additional beds fall far short of the NTC’s call for an around-the-clock “rapid access addiction clinic” and certified detox centre somewhere in Nuu-chah-nulth territory. That call came on the sixth anniversary of the public health emergency, in 2022, a year that Port Alberni saw double the fatalities by illicit drug use to the provincial average.
For Alice Sam, a cultural support worker with the Kuu-us Crisis Line Society, finding treatment facilities for her clients can seem almost impossible.
“I have three right now that I’ve been working with for the last three months to try and get them into treatment, try and get them into detox, and it’s like fighting a ghost,” said the Ahousaht member during the opioid forum. “People send me here, send me there.”
“When we do have people struggling and fighting, fighting for their own sobriety, let’s put the supports in place, before during and after,” added Sam. “People come out of treatment, where do they go?”
Dr. Shane Longman was another panelist at the forum, a Port Alberni physician whose practice specializes almost entirely on substance use. A critical tool for him is opioid agonist therapy, the prescribing of medical drugs that serve as a safer alternative to illicit substances. More nurses are being trained to prescribe these alternatives, and the options are growing to include things like Sublocade, an injected medication that works like Suboxone but stays in the body for 28 days.
But Longman cautioned that treatment differs for each person.
“An understanding of how individuals got to where they were, and where they want to be in the future is essential to being able to know how to tailor the approach to help that person,” he said. “That trauma and that pain is part and parcel of why people use. No one likes to be in pain, people want to be out of pain, and if they only know one or a couple ways of getting out of pain, eventually, they go back to using that.”
Meanwhile, the rest of society could be watching with guarded eyes. At the forum panelist Bijan Mahmoudi, a pharmacist in Port Alberni, spoke of the difficulties he has encouraging his staff to help someone who could, in some cases, be stealing from the store.
“We have stealing happening, but when that person becomes the person who’s using substances, that person stands out,” said Mahmoudi. “All my staff come to me a say, ‘Why do you have that person coming here? Why don’t you ban that person from the pharmacy?’ It puts me in a really, really bad position. Do I have to take care of my staff, or do I have to take care of my customer?”
It’s an illustration of the stigma attached to drug use, a challenge that British Columbia is trying to overcome by decriminalizing the possession of 2.5 grams of narcotics with a three-year Criminal Code exemption issued by Health Canada on Jan. 31.
Mahmoudi stressed that the crisis “needs ongoing attention from every corner.”
“There are so many factors involved that weren’t that person’s choice,” he said. “We’re not here to save the world, we’re here to save one person.”